ACUTE PANCREATITIS SECONDARY TO ALCOHOL CONSUMPTION WITH MINIMUM PLEURAL EFFUSION
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
A 30 year old male came to the opd with complaints of pain abdomen in the epigastric region, umbilical region,left hypochondric region relieved by sitting forward. H/O vomitings 2 episodes,non bilious,non projectile containing food particles Passing flatus + H/0 alcohol intake on Friday and Saturday. No other complaints
No h/o similar complaints in the past
No h/o DM,HTN,TB,Asthma, epilepsy,CVA,CAD
Personal history:
Appetite: normal
Diet:mixed
Bowel and bladder movements: regular
No known allergies
history of alcohol intake from 15 years , 180 ml per day , abstinence from 1 month.
CAGE criteria: score - 1
Have you ever felt you needed to Cut down on your drinking - no
Have people Annoyed you by criticizing your drinking - no
Have you ever felt Guilty about drinking - no
Have you ever felt you needed a drink first thing in the morning (Eye-opener) to steady your nerves or to get rid of a hangover - Yes
No significant family history
GENERAL EXAMINATION:
patient was examined in a well lit room after taking consent.
Patient is conscious, coherent and cooperative.
pallor - absent
icterus - absent
Cyanosis - absent
Clubbing - absent
No lymphadenopathy
No pedal edema.
Vitals:
Temperature: 98.2F
BP :170/90 mmHg
PR : 98bpm
RR: 22 cpm
SpO2 99% in room air
SYSTEMIC EXAMINATION:
CVS: S1 S2 heard
No thrills and murmurs
RS : trachea central
BAE- present
Normal vesicular Breath sounds
CNS: No focal neurological deficits
P/A : soft , non tender
Umbilicus - inverted
All quadrants moving equally with respiration
Scars- No scars seen
No palpable spleen and liver
Normal bowel sounds heard.
INVESTIGATIONS:
Heamogram:
Hemoglobin:17.8 gm/dl
Total count:10,500 cells/cumm
Platelet count:1.64 lakh/cumm
Blood urea:24 mg/dl
Liver function tests:
Total bilirubin-2.18 mg/dl
Direct bilirubin-0.83 mg/dl
AST-62 IU/L
ALT-28 IU/L
Alkaline phosphatase-112 IU/L
Total protein-55 gm/dl
Albumin-2.7 gm/dl
A/G ratio-0.98
Serum Amylase:1,244 IU/L
Serum creatinine:0.8 mg/dl
Serum electrolytes:
Sodium-137 mEq/L
Potassium-4.4 mEq/L
Chloride-98 mEq/L
Troponin I: negative
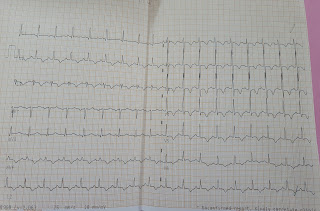
ECG:
CHEST X Ray:
TREATMENT:
DAY 1:
1.IVF-NS,RL @150 ml/hr
2.inj.pan 40mg iv/bd
3.nbm till further orders
4.inj.Tramadol 1 amp in 100 ml NS iv/bd
5.inj zofer 4mg iv/bd
6.strict bp,pr charting
7.strict i/o charting
8.ryle's tube insertion



Comments
Post a Comment